Uterine Fibroid Embolisation Fact Sheet
Uterine Fibroid Embolisation
Uterine Fibroid Embolisation is a procedure performed to eliminate the blood flow to Fibroids using x-rays and contrast (x-ray dye).
A specialist known as an Interventional Radiologist performs these procedures.
The contrast is injected through a thin plastic tube called a catheter, which is passed through a sheath inserted into the femoral artery.
Download PDFTo learn more about uterine fibroid embolisation, read our procedures page here.
Why do I need this procedure?
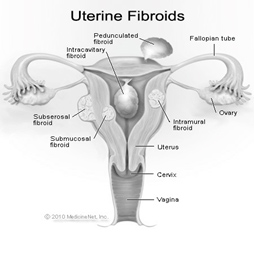
This procedure stops the blood supply to the fibroid(s) (non-cancerous growth) in the lining of the uterus, which often have the following symptoms;
- Heavy bleeding, anaemia, fatigue,
- Painful periods,
- Heavy sensation in the pelvis and back pain.
It is an alternative to surgical treatments such as a hysterectomy or myomectomy (a procedure which removes only the fibroid from the uterus).
It may also be a procedure that is done in combination with surgery. This will be discussed this with you at your appointment.
What should I expect?
- The procedure can take between 45-90mins.
- The contrast can cause a warm flushing or burning sensation. It only lasts for a few seconds and stops once the contrast has stopped being injected. Please ring MIVIR if you have a known allergy to Iodine or contrast.
- You may be required to take some time off work – please let the nurses know so they can organise a medical certificate for you. An attendance certificate can be provided for your carer.
- You will be required to stay overnight in hospital.
- We recommend you take the following week off work.
- It is not uncommon to experience flu like symptoms after the embolisation, this can last up to 5 days.
- Vaginal bleeding and discharge is common after the procedure and may only last a few days. Avoid using tampons during this time.
- Please contact MIVIR if you have any questions or concerns.
On the Day of your Procedure
You will need to present to the Day Procedure Unit on the day of your procedure – your admission time will be sent with your appointment confirmation. This will allow the nurses time to complete your admission paperwork and any other tests that may be required such as blood tests or pre-medication.
You will be required to fast for 4 hours before your procedure – this means no food or fluids. You may take any regular medication with a small sip of water. Please continue to take your blood pressure medication. Please bring all of your regular medications with you.
Please contact MIVIR if you are taking medication for the following;
- Diabetes,
- Stroke,
- Heart Conditions such as a Heart Attack or Atrial Fibrillation.
Useful Links
The following links also provide reliable information:
- Uterine Fibroid Embolisation – Inside Radiology
- Uterine Fibroid Embolization (UFE) – Radiology Info
- Uterine Fibroid Embolization – Fibroid Doc
- Uterine Artery Embolization – Johns Hopkins Medicine
Author: Dr John Vrazas
