Sclerotherapy for Varicose Veins Fact Sheet
What is Sclerotherapy?
Sclerotherapy is a procedure performed to treat vascular malformations. Vascular malformation is the name given to describe several different types of abnormal links between blood or lymph vessels.
These malformations are usually present at birth and tend to grow as the child develops. They are often asymptomatic (producing no symptoms) until adulthood. They may grow more rapidly due to hormonal changes or trauma around the area.
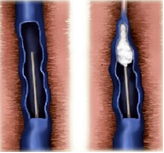
Injection of a sclerosant in a varicose vein
To learn more about sclerotherapy, read our procedures page here.
There are 2 ways to perform Foam Sclerotherapy;
- Direct injection of malformation.
- This can involve multiple injections of foam using ultrasound to visualise the malformation.
- Intravascular injection of malformation.
- This requires a femoral artery/vein puncture. Small catheters are directed to the malformation where the foam is injected directly into the malformation.
Your treatment options will be discussed with you on the day of your consultation.
Why do I need this procedure?
Foam sclerotherapy is performed to eliminate the flow/communication of blood/lymph between these abnormal structures. It is a treatment that is performed to provide symptomatic relief of the malformation, especially pain and swelling. It can also lighten areas of discolouration, especially on the face. It can be performed multiple times if necessary or in conjunction with surgery (if applicable).
What should I expect?
- The procedure can take between 60 – 90mins.
- The contrast can cause a warm flushing or burning sensation. It only last for a few seconds and stops once the contrast has stopped being injected. Please ring MIVIR if you have a known allergy to Iodine or contrast.
- You may be required to take some time off work – please let the nurses know so they can organise a medical certificate for you. An attendance certificate can be provided for your carer on the day of the procedure.
- Please make sure you have someone to pick you up after your procedure. You procedure will be cancelled if you don’t have an escort. Please contact MIVIR as soon as possible if this cannot be arranged.
- After the procedure you may experience mild-moderate discomfort which should resolve over the following few days. You should only require oral pain medication to help relieve symptoms. Ice, rest and elevation can also provide relief.
On the day of your Procedure
You will need to present to the Day Procedure Unit on the day of your procedure – your admission time will be sent to you with your appointment time. This will allow the nurses time to complete your admission paperwork and any other tests that may be required such as blood tests or pre-medication.
You will be required to fast for 4 hours before you procedure – this means no food or fluids. You may take any regular medication with a small sip of water. Please continue to take your blood pressure medication. Please bring a list of your medications with you.
Please contact MIVIR if you are taking medication for the following;
- Diabetes,
- Stroke,
- Heart Conditions such as a Heart Attack or Atrial Fibrillation.
Useful Links
Author: Dr John Vrazas
